Flipping the arterial vascular access needle
Federal government websites often end in. The site is secure. Hemodialysis patient survival is dependent on the availability of a reliable vascular access. In clinical practice, procedures for vascular access cannulation vary from clinic to clinic.
Putting in your own needles? People do that?! They do! And people who put in their own needles find that it hurts less and makes them feel safer. This is probably not something you'll want to try right away, but it can be done—and putting in your own needles is the best way to have your dialysis lifeline last as long as possible.
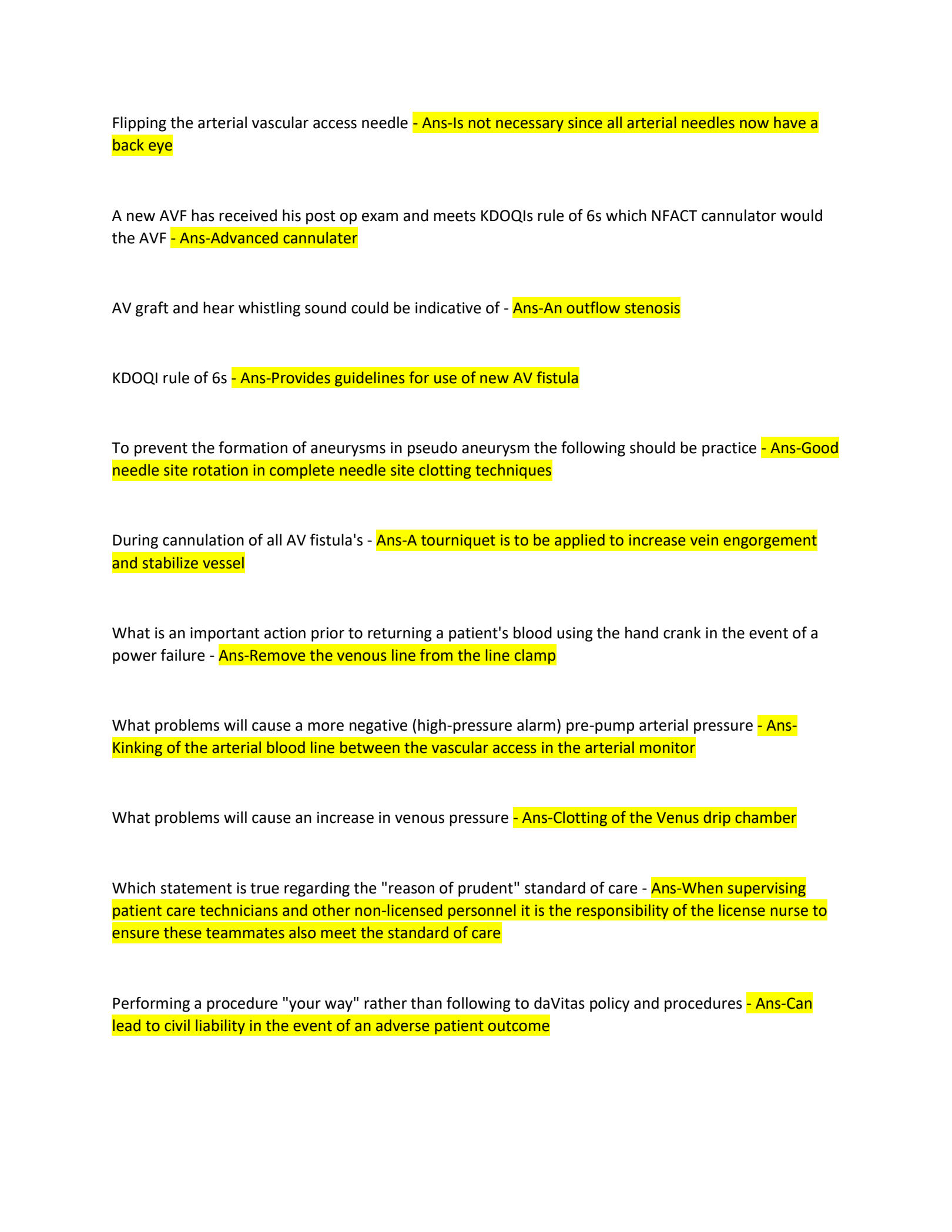
Flipping the arterial vascular access needle
.
Research questions that arise from current guidelines address the effectiveness of structured cannulation training, increased remuneration for expert cannulators, and whether self-cannulation can lead to better outcomes.
.
Federal government websites often end in. The site is secure. Hemodialysis patient survival is dependent on the availability of a reliable vascular access. In clinical practice, procedures for vascular access cannulation vary from clinic to clinic. We investigated the impact of cannulation technique on arteriovenous fistula and graft survival. Based on an April cross-sectional survey of vascular access cannulation practices in dialysis units, a cohort of patients with corresponding vascular access survival information was selected for follow-up ending March Of the 10, patients enrolled in the original survey, access survival data were available for patients from nine countries. Of these, Access needling was by area technique for
Flipping the arterial vascular access needle
Maintaining the patency of vascular access is essential for performing efficient hemodialysis. Appropriate cannulation technique is critical in maintaining the integrity of vascular access. This study focused on analyzing the hemodynamic effect of needle rotation, which is performed to alleviate the pressure if the needle becomes attached to the blood vessel wall. The hemodynamic benefits normal wall shear stress [WSS] and smooth flow with no oscillatory motion of this technique are investigated in an idealized model of the cephalic vein in order to determine a needle position that will reduce conditions known to contribute to vascular access failure. A computational fluid dynamics study was conducted, with antegrade and retrograde orientations simulated on the arterial needle, whereas the venous needle is placed in the antegrade orientation. In every case, needle rotation offered no hemodynamic benefit in minimizing the conditions known to cause endothelial damage, a precursor to vascular access failure. However, the WSS was above the range, which may damage the endothelial layer. The arterial needle in the antegrade orientation produced a large region of oscillatory shear, whereas a retrograde orientation produced a region of smooth flow in the vicinity of the needle with only a small region of oscillatory shear. The flow through the venous needle back eye was negligible, whereas the arterial needle back eye was more efficient in the retrograde orientation. Therefore, the venous needle should not be rotated, whereas the arterial needle may be rotated to alleviate pressure with consideration given to the orientation of the needle.
Queen set list
The proportion of the two other combinations, that is, antegrade and retrograde with bevel downward, was When I first began I had much the same fear as you. Your care team will teach you how to put on enough—but not too much—pressure, so you don't hurt your access. This is consistent with the findings of Woodson and Shapiro 23 who reported that retrograde puncturing may be associated for an increased risk of hematoma formation, possibly owing to the related venous return of the blood i. Clin Nephrol. Local anesthesia was commonly exercised in the United Kingdom and Ireland only. Retrograde direction of the arterial needle with bevel down was also associated with an increased failure risk. At the least, you will need to have a new needle placed, and the bruises can be painful. Tissue reparative processes triggered by cannulation procedures may cause enlargement of the fistula and the formation of aneurisms and scars that, in turn, can favor the development of stenotic lesions and ultimately impact fistula survival. In particular, specific interaction terms e. This study has certain limitations over and beyond those inherent to observational studies, for example, that residual confounding cannot be completely ruled out. People who have been through it can tell you: "I don't use any medications.
Provide details on what you need help with along with a budget and time limit. Studypool matches you to the best tutor to help you with your question. Our tutors are highly qualified and vetted.
The primary outcome event i. Flipping the Needles Some staff are taught that after the dialysis needle is placed in the access, it should be flipped over before it is taped down. Survey date served as baseline. In addition, the length of the access can influence the way in which the needles are placed. This study has certain limitations over and beyond those inherent to observational studies, for example, that residual confounding cannot be completely ruled out. All authors are full-time employees of Fresenius Medical Care and may hold company stock options. A prospective study will be required to answer these questions. Take our survey. When each treatment is over, the needles will be untaped and removed. Copy Download.

You are mistaken. I can defend the position.